HHC, which stands for Home Health Care, refers to a range of medical and non-medical services provided to individuals in their own homes to promote health, independence, and quality of life. HHC encompasses a wide array of services, including skilled nursing, physical therapy, occupational therapy, speech therapy, personal care assistance, and medical social work. These services are typically delivered by trained professionals, such as registered nurses, therapists, home health aides, and social workers, under the supervision of a physician or other healthcare provider. HHC plays a critical role in supporting individuals recovering from illness or injury, managing chronic conditions, and facilitating aging in place for older adults.
1. Types of Services Offered:
HHC encompasses a broad spectrum of services tailored to meet the diverse needs of individuals receiving care in their homes. Skilled nursing services may include wound care, medication management, infusion therapy, and monitoring of vital signs. Physical therapy focuses on improving mobility, strength, and balance through therapeutic exercises and interventions. Occupational therapy helps individuals regain independence in activities of daily living, such as dressing, grooming, and meal preparation. Speech therapy addresses communication and swallowing disorders, while medical social work provides counseling, advocacy, and assistance with navigating community resources.
2. Benefits of Home Health Care:
HHC offers several advantages over institutional care settings, such as hospitals or nursing homes. By receiving care in the comfort and familiarity of their own homes, individuals can maintain a sense of independence, autonomy, and dignity. HHC promotes continuity of care and personalized attention, with services tailored to meet the unique needs and preferences of each individual. Additionally, HHC can reduce the risk of hospital readmissions and healthcare-associated infections, leading to improved health outcomes and cost savings for patients, families, and payers.
3. Eligibility Criteria and Referral Process:
To qualify for HHC services, individuals typically need a referral from a physician or other healthcare provider, who assesses their medical condition and determines the appropriate level of care. Eligibility criteria may vary depending on the specific services needed and the requirements of insurance payers, such as Medicare or Medicaid. Common eligibility criteria include being homebound or having difficulty leaving the home without assistance, requiring skilled nursing care or therapy services, and having a medical condition that necessitates ongoing monitoring or treatment.
4. Payment and Reimbursement:
HHC services are reimbursed through various sources, including government programs, private insurance plans, and out-of-pocket payments. Medicare, the federal health insurance program for older adults and individuals with disabilities, covers HHC services for eligible beneficiaries who meet certain criteria, such as being homebound and requiring skilled care on an intermittent basis. Medicaid, the joint federal-state program for low-income individuals, also covers HHC services for eligible beneficiaries, although coverage and eligibility criteria may vary by state. Private insurance plans may offer coverage for HHC services as part of their benefits packages, with reimbursement rates and coverage levels determined by individual plans.
5. Regulatory Oversight and Quality Assurance:
HHC agencies are subject to regulatory oversight and quality assurance measures to ensure the safety, effectiveness, and quality of care provided to individuals in their homes. In the United States, HHC agencies must comply with federal and state regulations, including licensure requirements, certification standards, and participation in quality reporting initiatives. Regulatory agencies, such as the Centers for Medicare & Medicaid Services (CMS) and state departments of health, conduct surveys, inspections, and audits to assess compliance with regulatory requirements and enforce standards of care.
6. Interdisciplinary Care Teams:
HHC services are typically delivered by interdisciplinary care teams composed of various healthcare professionals working together to coordinate and deliver comprehensive care to individuals in their homes. These teams may include registered nurses, licensed practical nurses, physical therapists, occupational therapists, speech therapists, home health aides, medical social workers, and other professionals, depending on the specific needs of the individual receiving care. Interdisciplinary collaboration and communication are essential for optimizing care coordination, ensuring continuity of care, and addressing the holistic needs of individuals and their families.
7. Role of Caregivers and Family Members:
Caregivers and family members play a crucial role in supporting individuals receiving HHC services, providing emotional support, assistance with activities of daily living, and coordination of care. Caregivers may receive training and education from HHC agencies to help them effectively manage the needs of their loved ones and ensure the safety and well-being of all parties involved. Effective communication between caregivers, family members, and healthcare professionals is essential for promoting collaboration, addressing concerns, and facilitating optimal outcomes for individuals receiving care at home.
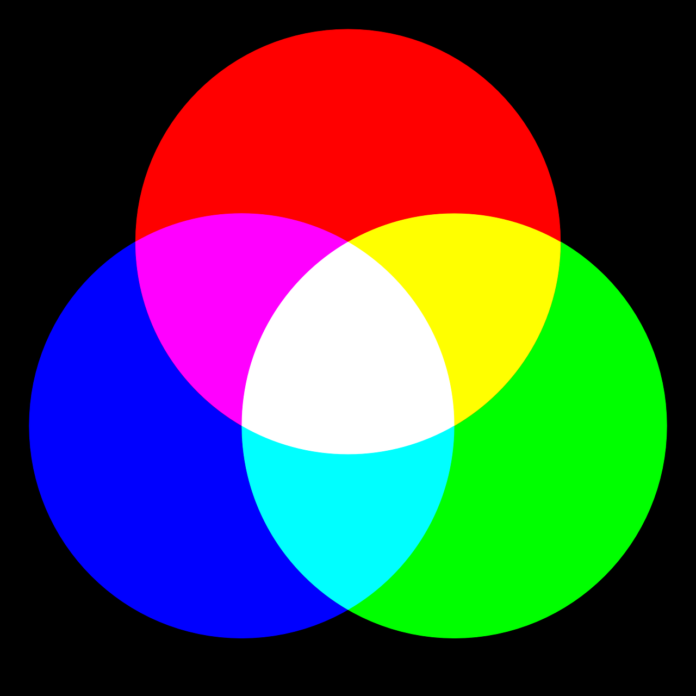
8. Technology and Innovation in Home Health Care:
Advancements in technology and innovation are transforming the delivery of HHC services, enabling remote monitoring, telehealth consultations, and electronic health record documentation. Telehealth platforms allow healthcare providers to conduct virtual visits with individuals receiving HHC services, providing real-time assessments, consultations, and education without the need for in-person appointments. Remote monitoring devices, such as wearable sensors and smart home technologies, enable healthcare providers to track vital signs, medication adherence, and activity levels, facilitating early detection of health changes and proactive interventions.
9. Evolving Models of Care Delivery:
In response to changing healthcare needs and advancements in technology, the home health care sector is witnessing the emergence of new models of care delivery aimed at improving access, efficiency, and outcomes. These models may include innovative approaches such as mobile health clinics, community-based care coordination programs, and collaborative partnerships between healthcare organizations and community-based organizations. By leveraging community resources, technology-enabled solutions, and interdisciplinary collaboration, these models seek to address social determinants of health, enhance care coordination, and improve health outcomes for individuals receiving care at home.
10. Future Directions and Challenges:
As the demand for home health care continues to grow, the sector faces several challenges and opportunities for future development. Key challenges include workforce shortages, reimbursement pressures, regulatory compliance, and access to technology and infrastructure in underserved communities. Additionally, the aging population, rising prevalence of chronic diseases, and shifting healthcare landscape necessitate ongoing innovation and adaptation within the home health care sector. Future directions may include greater integration with primary care and specialty services, expansion of telehealth and remote monitoring capabilities, and enhanced collaboration with community partners to address social determinants of health.
Conclusion: Home Health Care (HHC) plays a vital role in supporting individuals of all ages to receive comprehensive medical and non-medical services in the comfort and familiarity of their own homes. With a wide range of services tailored to meet individual needs, HHC promotes independence, autonomy, and quality of life for patients while reducing the risk of hospital readmissions and healthcare-associated infections. By leveraging interdisciplinary care teams, regulatory oversight, and technological innovations, HHC agencies strive to deliver high-quality, patient-centered care that meets the evolving needs of individuals and families in their communities